This story is part of The Salt Lake Tribune’s ongoing commitment to identify solutions to Utah’s biggest challenges through the work of the Innovation Lab. [ Subscribe to our newsletter here ] Utah’s population boom has contributed to growth-related tension, a housing shortage and — one industry leader says — a lower rate of hospital beds per capita than nearly every other state in the country. The state has about 193 beds of any sort — from brief surgery recovery to overnight stays to critical care —available for hospital patients per 100,000 people, according to data from The Cecil G.
Sheps Center for Health Services Research at The University of North Carolina at Chapel Hill and the U.S. Census Bureau.

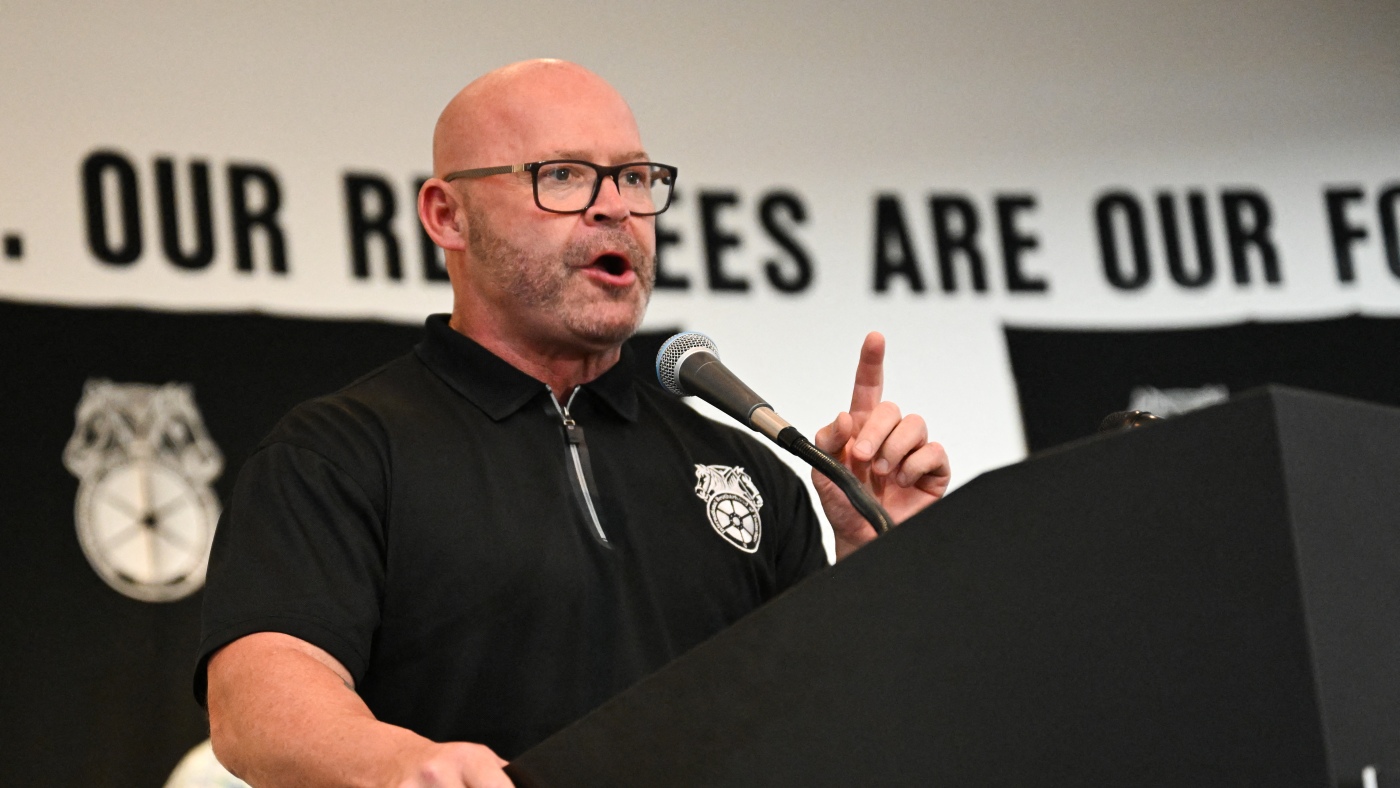
The state’s rapid population growth has outpaced hospitals’ ability to add beds, said Francis Gibson, CEO of the Utah Hospital Association. “You can’t just throw up a hospital because the population has grown,” he said. There are some mitigating factors, Gibson said, including the Beehive State’s generally younger and healthier population, gains in telemedicine and more surgeries that don’t require an overnight stay.
Hospitals and their parent health systems are still working to add capacity and resources, he said, including new hospitals and expansions at existing facilities. Though Utah’s growth has slowed some in recent years, it’s still higher than most other states. People talk about connections between that boom and the housing shortage , but it’s even harder for health systems to keep up with growth, Gibson said.
Building a home costs about $200 to $300 per square foot, he said, compared to $2,500 to $4,000 a square foot to build a hospital. Health systems can’t be as “mobile and adaptable to a booming population” as developers, he said. In 2016, Utah had a population of about 3 million and 4,890 hospital beds, based on Sheps Center and Census Bureau data.
The state’s population was up to 3.4 million people as of last July with 6,593 hospital beds, according to the same sources. Though the state’s rate of hospital beds increased from about 161 to 192.
9 per 100,000 people, it remained lower than nearly every state in the country. In 2016, Utah’s rate was lower than that of every state except Hawaii. Last year, it was the third lowest, with Washington falling behind and Hawaii’s rate remaining lower than Utah’s.
That’s despite Utah tying for 32nd with 1.7 hospitals per 100,000 people. Many of Utah’s hospitals have fewer than 100 beds, based on Sheps Center data, including ones in cities.
Other than specialty hospitals, the smallest are in rural areas. Those rural hospitals, though, are “pretty dang good,” Gibson said. They’re able to draw specialists for a couple of days a month or longer if they have housing available, he said, and telemedicine has been a “game-changer” for improving residents’ ability to access a specialist without driving several hours .
That isn’t to say hospitals aren’t adding beds and finding ways to decrease the need for lengthy stays. University of Utah Health has been working to build a hospital complex in West Valley City since at least 2022. The system plans to break ground in early 2025 and phase construction on the project at 3750 South and 5600 West.
The medical campus will start with a multispecialty outpatient center coming first in 2027. It will have an emergency department, exam rooms and some specialty care, like a facility for heart care. Hospital rooms will come later, but officials have not specified any dates.
In downtown Salt Lake City, Intermountain Health plans to build a new hospital on the block of State Street that’s now an open pit where Sears once sat . Making the proposal come to life will require city officials to green-light two zoning changes, but Salt Lake City City Council members have so far been disappointed that the health care system’s plans don’t include more ways to activate foot traffic along State Street. And they recently said they will make the Utah-based hospital chain sign a development agreement to regulate how the huge new medical facility will be built to interact with surrounding homes and businesses around Main and State streets between 700 South and 800 South.
Wish list items include more ground-floor amenities such as open spaces, walkways, a food market, a coffee shop and other community resources. Intermountain also recently broke ground to add a new operating room and pharmacy services to Garfield Memorial Hospital in Panguitch. The changes will allow for surgeries that couldn’t happen because an older operating room didn’t have proper ventilation for anesthesia gas.
Garfield County residents typically have to travel far for certain procedures like a tonsillectomy, said DeAnn Brown, president of Intermountain Garfield Memorial Hospital. “Now they get to stay close to home, near their families, making their care more convenient and comfortable,” Brown said in a statement about the hospital expansion . Health systems will continue to add resources where needed, Gibson said, but they’re also working to decrease the need for hospital beds.
“Hospitals are looking to see how we can shorten your stay,” the UHA executive said. About 80% of surgeries can be done in an outpatient surgery setting, Gibson said. Outpatient surgeries, also called same-day or ambulatory surgeries, often are cheaper.
Typical examples of outpatient surgeries are mole removal, hernia repair and knee replacement. Hospitals also free up beds more quickly, Gibson said, adding people heal better at home than in an “uncomfortable hospital bed.” Gibson also said hospitals are trying to look at Utah’s future health care needs, especially as Utah’s population ages and focus shifts from healthy living to healthy aging.
Megan Banta is The Salt Lake Tribune’s data enterprise reporter, a philanthropically supported position . The Tribune retains control over all editorial decisions..