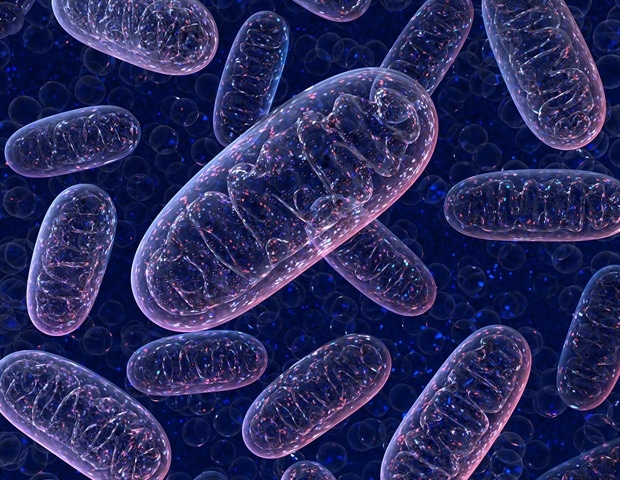
Mitochondria are crucial organelles for cellular homeostasis, regulating processes such as ATP production, reactive oxygen species (ROS) management and Ca 2+ signaling. In particular, mitochondrial Ca 2+ plays a dual role: enabling physiological functions like metabolism and ATP synthesis while contributing to pathological processes such as apoptosis and oxidative stress when dysregulated. The balance of mitochondrial Ca 2+ is maintained through interactions between uptake and efflux mechanisms.
Key players in the process include the mitochondrial calcium uniporter (MCU) complex for Ca 2+ influx and the Na + /Ca 2+ exchanger (NCLX) for efflux. The mitochondria-endoplasmic reticulum contact sites (MERCS) also play a pivotal role in facilitating Ca 2+ transfer. Dysregulation at any level, such as excessive uptake or impaired efflux, leads to mitochondrial Ca 2+ overload, triggering ROS production, mitochondrial membrane potential loss, and permeability transition pore activation, which can culminate in cell death.

A review by a team of researchers at the Chinese Academy of Science highlights the role of mitochondrial Ca 2+ imbalance in neurodegenerative diseases, including Alzheimer's disease (AD), Parkinson's disease (PD), Huntington's disease (HD), amyotrophic lateral sclerosis (ALS), and spinocerebellar ataxias (SCAs). In AD, amyloid-beta (Aβ) disrupts mitochondrial Ca 2+ homeostasis by enhancing Ca 2+ uptake via MCU and impairing efflux through NCLX. These changes lead to ROS accumulation, energy depletion, and neuronal death.
MERCS alterations exacerbate the pathology by increasing ER-mitochondria Ca 2+ transfer. In PD, α-synuclein aggregates disrupt MERCS, impairing Ca 2+ transfer from the ER to mitochondria, while DJ-1 mutations reduce the antioxidant capacity, exacerbating oxidative stress. Mutations in several ALS-associated genes, including TAR DNA-binding protein 43 (TDP-43), superoxide dismutase 1 (SOD1), and C9orf72, have been reported to physically interact with the mitochondria and play pivotal roles in maintaining mitochondrial function.
Meanwhile, HD is caused by the expansion of CAG repeats in the huntingtin (HTT) gene, producing mutant huntingtin (mHTT) protein. In HD, mHTT increases the sensitivity of IP 3 R and NMDA receptors , causing abnormal cytosolic/mitochondrial Ca 2+ signaling and mitochondrial dysfunction. As for SCAs, they are a group of inherited neurodegenerative disorders caused by polyglutamine expansions in genes such as ATXN2 and ATXN3.
Mutant proteins enhance IP 3 R-mediated Ca 2+ release from the ER, resulting in excessive mitochondrial Ca 2+ uptake and impaired efflux. The review, published in the KeAi journal Mitochondrial Communications , also discusses the potential interventions targeting mitochondrial Ca 2+ regulators. Strategies include modulating MCU and NCLX activity, stabilizing MERCS, and developing compounds that prevent mitochondrial Ca 2+ overload.
For instance, inhibitors of MCU and stabilizers of mitochondrial permeability transition pore (mPTP) show promise in preclinical models. In this review, we emphasize the role of Ca 2+ mit o in both physiological and pathophysiological contexts. Developing drugs that specifically target parts of the MCU complex, NCLX, or MERCS is tricky.
Hence, we need sufficient information to ensure they only affect mitochondrial Ca 2+ levels where needed, without messing up the healthy tissues". Tie-Shan Tang, corresponding author KeAi Communications Co., Ltd.
Sun, J., et al . (2025).
Decoding the influence of mitochondrial Ca2+ regulation on neurodegenerative disease progression. Mitochondrial Communications . doi.
org/10.1016/j.mitoco.
2025.01.001 .
.















