65 people from 9 states have gotten sick from the same strain of Salmonella. The 9 states include the 3 states where the eggs were sold – Illinois, Michigan, and Wisconsin – in addition to California, Colorado, Iowa, Minnesota, Utah, and Virginia. Most sick people are from Wisconsin (42) or Illinois (11).
24 people have been hospitalized and no deaths have been reported. This outbreak may be difficult to treat with some commonly recommended antibiotics and may require a different antibiotic choice for people who need them. Laboratory testing showed that the Salmonella making people sick is resistant to nalidixic acid and ciprofloxacin.

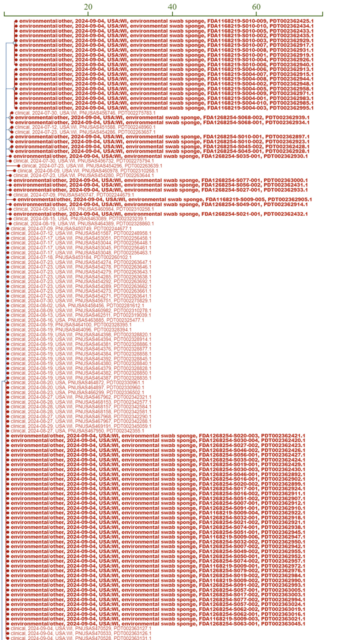
This may make illnesses in this outbreak difficult to treat with some commonly recommended antibiotics and may require a different antibiotic choice for people who need them. Data show that eggs supplied by Milo’s Poultry Farms LLC are contaminated with Salmonella and are making people sick. FDA inspected Milo’s Poultry Farms and collected samples.
FDA’s analysis showed the outbreak strain of Salmonella was found in the packing facility and the hen egg laying house. On September 6, Milo’s Poultry Farms LLC recalled eggs. Recalled eggs were sold to stores and restaurants in Illinois, Michigan, and Wisconsin, and labeled with “Milo’s Poultry Farms” or “Tony’s Fresh Market.
” All egg types, sizes and expiration dates are recalled. A whole lot of clinical and environmental WGS: What is Salmonella? There are two Salmonella species: Salmonella enterica ( S. enterica ) and Salmonella bongori ( S.
bongori ). S. bongori strains predominantly colonize cold-blooded reptiles, whereas S.
enterica strains are capable of infecting both humans and mammals. [1] Based on factors such as morphology, structure, mode of reproduction, and other criteria, the two species are further classified into subgroups called serotypes or serovars. More than 2,600 serotypes have been described for Salmonella , and they are characterized by the type(s) of animal they are found in or by the clinical symptoms they cause.
[2] Of these, less than 100 are responsible for most human Salmonella infections. [3] Where Does Salmonella Come From? Salmonellae are widely distributed in nature and are found in the intestinal tract of wild and domesticated animals and in humans. Salmonella poisoning can occur when a person ingests contaminated fecal particles transmitted by another infected human or animal.
[4] Salmonella enterica serotypes Typhi, Sendai, and Paratyphi A, B, or C are found exclusively in humans. These serotypes, collectively referred to as typhoidal Salmonella , cause enteric fever (also known as typhoid or paratyphoid fever if caused by serotypes Typhi or Paratyphi, respectively). [5] Most often, enteric fever is acquired through ingestion of food or water contaminated with human feces.
Most U.S. residents who are diagnosed with typhoidal Salmonella are infected while traveling abroad in areas where typhoid fever and paratyphoid fever are common.
Three types of vaccines against S. Typhi are commercially available, although there is still not a single licensed vaccine available against S. Paratyphi A.
[6] Persons planning to travel outside of the United States are advised to find out if a vaccine for typhoid fever is recommended ( see www.cdc.gov/travel ).
Most Salmonella infections are caused by eating contaminated food. One study found that 87% of all confirmed cases of Salmonella are foodborne. Foods of animal origin, including meat, poultry, eggs, or dairy products can become contaminated with Salmonella .
Eating uncooked or inadequately cooked food—or food cross contaminated with uncooked or undercooked products—can lead to human infections. As explained in a comprehensive report issued by the U.S.
Department of Agriculture’s Economic Research Service: Salmonella contamination occurs in a wide range of animal and plant products. Poultry products and eggs are frequently contaminated with S. Enteritidis, while beef products are commonly contaminated with S.
Typhimurium. Other food sources of Salmonella may include raw milk or other dairy products and pork. In the past two decades, consumption of produce, especially sprouts, tomatoes, fruits, leafy greens, nuts, and nut butters, has been associated with Salmonella illnesses.
[7] The surface of fruits and vegetables may be contaminated by human or animal feces. Changes in food consumption and production, as well as the rapid growth of international trade in agricultural products, have facilitated the transmission of Salmonella associated with fresh fruits and vegetables. In the United States, Salmonella is the second most commonly isolated bacterial pathogen when laboratory diagnosis of diarrhea is sought.
[8] However, passive laboratory surveillance, which uses voluntary reporting by health care providers and facilities, captures only a fraction of illnesses that actually occur. Furthermore, only a small proportion of illnesses are confirmed by laboratory testing and reported to public health agencies. Thus, researchers rely on quantitative statistical modeling to estimate the incidence of foodborne illness.
These estimates are used to direct policy and interventions. What are the Symptoms of Salmonellosis? Salmonella infections can produce a broad range of disease, from no symptoms to severe illness. The most common clinical presentation is acute gastroenteritis.
Symptoms commonly include diarrhea and abdominal cramps, often accompanied by fever of 100°F to 102°F (38°C to 39°C). More serious infections may also involve bloody diarrhea, vomiting, headache, and body aches. [9] The incubation period, or the time from ingestion of the bacteria until the symptoms start, is generally 6 to 72 hours; however, there is evidence that in some situations the incubation can be longer than 10 days.
People with salmonellosis usually recover without treatment within three to seven days. Nonetheless, Salmonella bacteria can persist in the intestinal tract and stool for many weeks after the resolution of symptoms—on average, one month in adults and longer in children. [10] Treatment of Salmonellosis S.
Typhi and S. Paratyphi are capable of causing systemic illness if they invade the bloodstream (termed “bacteremia”). “Septicemia” or “sepsis” (bloodstream infection or “blood poisoning”) occurs if the bacteria multiply in the blood and cause the immune system to respond by activating inflammatory mechanisms.
This may result in the development of “systemic inflammatory response syndrome,” or “SIRS.” By definition, SIRS includes tachycardia, tachypnea, fever, and abnormal white blood cell count. When the bacteria involved are S.
Typhi or S. Paratyphi, this serious illness is called enteric typhoid, or paratyphoid fever. Symptoms may start gradually and include fever, headache, malaise, lethargy, and abdominal pain.
In children, it can present seemingly innocuously as a non-specific fever. The incubation period for S. Typhi is usually 8 to 14 days, but it can range from three to 60 days.
For S. Paratyphi infections, the incubation period is similar to that of nontyphoidal Salmonella —one to 10 days. [11] Medical treatment is acutely important, though, if the patient becomes severely dehydrated or if the infection spreads from the intestines.
Persons with severe diarrhea often require re-hydration, usually with intravenous (IV) fluids. But antibiotics are not necessary or indicated unless the infection spreads from the intestines, at which time the infection can be treated with ampicillin, gentamicin, trimethoprim/sulfamethoxazole, or ciprofloxacin. Unfortunately, though, some Salmonella bacteria have become resistant to antibiotics, largely as a result of the use of antibiotics to promote the growth of feed animals.
[12] [1] Hernandez, A. K. C.
Salmonella bongori . Poultry and Avian Diseases. Encyclopedia of Agriculture and Food Systems .
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/salmonella-bongori.
[2] Boore AL, et al . (2015). Salmonella enterica Infections in the United States and Assessment of Coefficients of Variation: A Novel Approach to Identify Epidemiologic Characteristics of Individual Serotypes, 1996–2011.
PloS One . 10(12): e0145416 [3] Besser JM. (2018).
Salmonella epidemiology: a whirlwind of change. Food Microbiol . 71:55-9.
[4] Chiu, C.-H. (2019).
Salmonella, Non-Typhoidal Species (S. Choleraesuis, S. Enteritidis, S.
Hadar, S. Typhimurium) . http://www.
antimicrobe.org/b258.asp.
[5] Ohad eGal-Mor, Erin C Boyle, & Guntram A. Grassl. (2014).
Same species, different diseases: how and why typhoidal and non-typhoidal Salmonella enterica serovars differ. Frontiers in Microbiology , 5. https://doi.
org/10.3389/fmicb.2014.
00391 [6] Id. [7] National Typhoid and Paratyphoid Fever Surveillance Annual Summary, 2015.” Centers for Disease Control and Prevention, 6 Nov.
2018. Available at: https://www.cdc.
gov/typhoid-fever/reports/annual-report-2015.html . [8] “National Enteric Disease Surveillance: Salmonella Annual Report, 2016.
” Centers for Disease Control and Prevention, 28 Feb. 2018. Available at: https://www.
cdc.gov/nationalsurveillance/pdfs/2016-Salmonella-report-508.pdf .
[9] “ Salmonella .” Centers for Disease Control and Prevention, 24 Jun. 2020.
Available at: https://www.cdc.gov/salmonella/ .
[10] Id. [11] Miller, S. and Pegues, D.
“ Salmonella Species, Including Salmonella Typhi” in Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, Sixth Edition, Chap. 220, pp. 2636-50 (2005).
[12] Medalla, F., Gu, W., Mahon, B.
E., Judd, M., Folster, J.
, Griffin, P. M., & Hoekstra, R.
M. (2016). Estimated Incidence of Antimicrobial Drug-Resistant Nontyphoidal Salmonella Infections, United States, 2004-2012.
Emerging infectious diseases , 23 (1), 29–37. https://doi.org/10.
3201/eid2301.160771.