Vijay K. Kuchroo, PhD, DVM, of the Gene Lay Institute of Immunology and Inflammationof Brigham and Women’s Hospital, Massachusetts General Hospital and Harvard Medical School and the Ann Romney Center for Neurologic Diseases at Brigham and Women’s Hospital, is the co-corresponding author of a paper published in Nature, “Neuropeptide signaling orchestrates T cell differentiation.” How would you summarize your study for a lay audience? T helper (TH) cells are essential immune cells that help other immune cells function effectively.
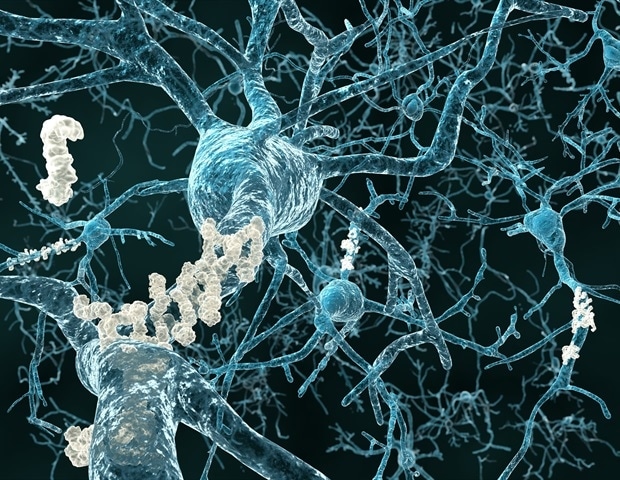
When activated in response to environmental stimuli, these cells can differentiate into either TH1 cells, which fight against viruses and intracellular pathogens, or TH2 cells, which fight against extracellular pathogens like bacteria and parasites. However, scientists haven't fully understood whether infected tissue itself has any role in directing the optimal T cell differentiation in response to tissue infection. Our research has shown that virally infected neurons play a significant role by promoting the development of TH1 cells and inhibiting TH2 cells during viral infections.
This communication between infected neurons and the immune system happens through molecules called neuropeptides, which interact with specific receptors on T cells to guide their fate. This process is crucial for the body to effectively control viral infections. What knowledge gap does your study help to fill? Our findings show that neuroimmune communication plays a crucial role in determining T cell fate, establishing a novel link between infected tissue (neurons) and the differentiation of T cell subsets.
What methods or approaches did you use? Our team investigated the regulatory mechanisms that guide the optimal differentiation of T cells into specific lineages while inhibiting others. To do this, we used a technique called single-cell RNA sequencing (scRNA-seq) to study how genes are expressed over time, looking at two types of immune cells (TH1-TH2) in a cell culture system. We also applied CRISPR screening to identify which regulators help control T cell fate development into Th1 vs.
Th2 cells. Related Stories Patient-derived organoids: Transforming cancer research and personalized medicine Research suggests no need for yellow fever vaccine booster after initial dose Scientists develop first durable human lip cell models in the lab By combining various gene and and cellular biology techniques, we demonstrated that the neuropeptide receptor RAMP3 plays a key role in how T cells develop using preclinical models. What did you find? We showed that neuroimmune circuits, influenced by neuropeptides and theirreceptors, play a pivotal role in determining T cell fate.
We also explored how neuropeptides ensure optimal T cell differentiation and drive robust antiviral responses. What are the implications? Our study suggests that changes to neuroimmune circuits may help balance different types of T cell and lead to better immune responses. For example, previous research has shown an imbalance of TH2 differentiation over TH1 is correlated with increased death in patients with COVID-19.
Targeting the neuroimmune pathways that regulate T cell fate decisions may offer new therapeutic opportunities for patients with severe COVID-19 infections, cancer and other autoimmune diseases. Brigham and Women's Hospital Hou, Y., et al .
(2024). Neuropeptide signalling orchestrates T cell differentiation. Nature .
doi.org/10.1038/s41586-024-08049-w .
.