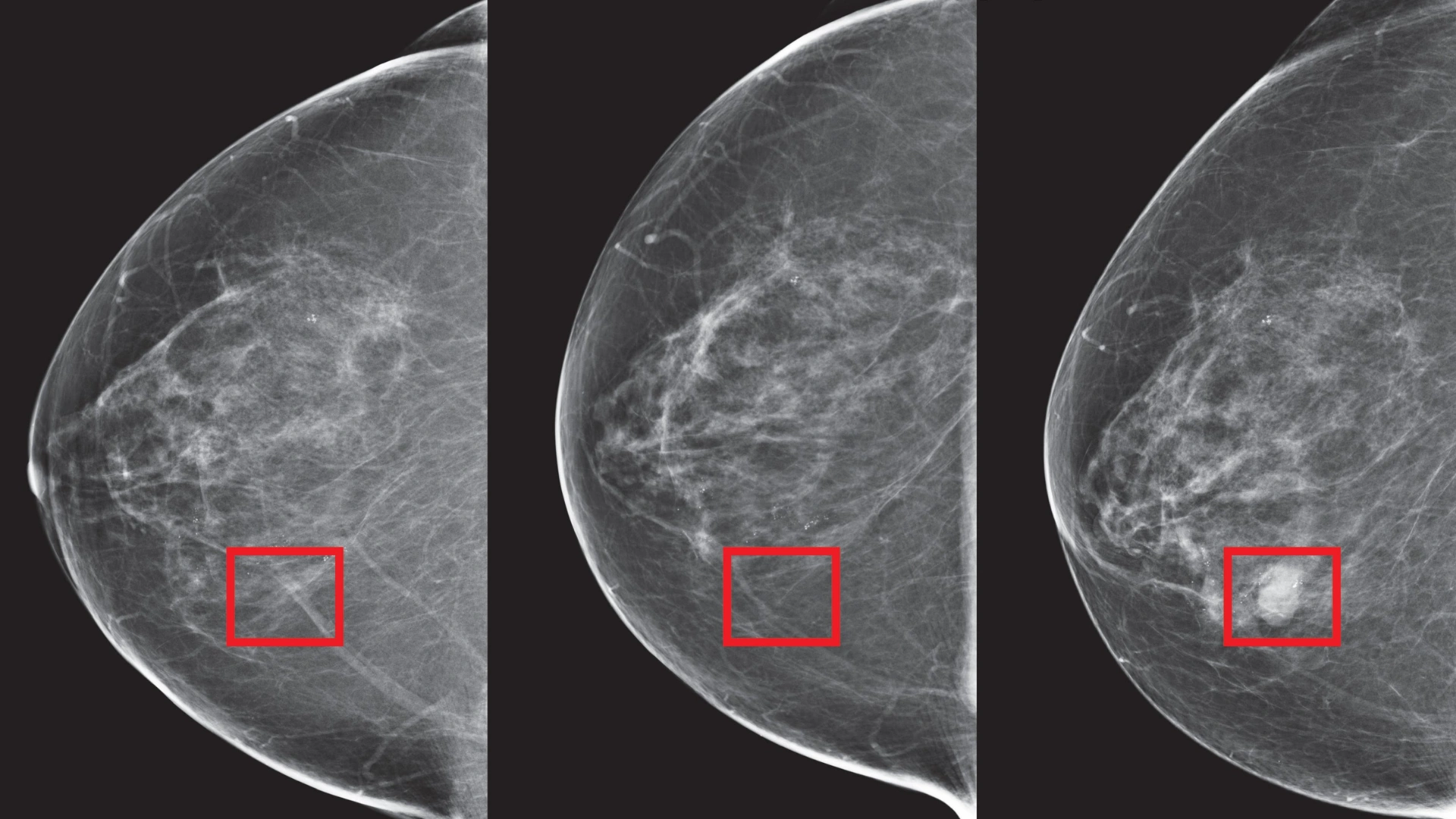
MIT researchers have developed Mirai , an advanced AI model that can detect breast cancer up to five years before a clinical diagnosis. But how can it detect cancer? It uses deep learning algorithms and analyzes mammography images, through which it makes accurate predictions of precancerous changes in breast tissue. What sets Mirai apart is its ability to identify invasive cancer cells in tissue that appears normal, offering the potential for earlier and more effective treatments.
This breakthrough could significantly improve survival rates, especially for women at high risk of developing breast cancer. Why Early detection is life saving Early detection is a critical weapon in the battle against breast cancer. For decades, mammography has played a major role in the screening process but, unfortunately, does not capture the early disease very well in at-risk patients.

Mirai addresses this gap with much more precise predictions, risk assessments, and earlier intervention. It predicts the risk of breast cancer by combining demographic factors like age and family history with deep learning techniques. It would examine patterns within mammography images to identify changes in the breast that are abnormal even before they become clinically detectable.
In this sense, it has the potential to redefine the future of early detection and ultimately better patient outcomes. What makes Mirai stand out, however, is its performance across the wide range of populations. The researchers tested Mirai on screening data from seven hospitals in five countries: the United States, Israel, Sweden, Taiwan, and Brazil.
Among these institutions are the world-class medical centers such as Massachusetts General Hospital (MGH), Novant Health, and Karolinska University Hospital, among others. On these test sets, Mirai showed its performance in the prediction of breast cancer risk over a five-year horizon. The performance of the AI model was better than that of the traditional risk models, such as the Tyrer-Cuzick (TC) model, which is in use in clinical practice.
For instance, on the MGH test set, Mirai had an AUC of 0.76, whereas the TC model had only 0.62.
This advance indicates a significant capability in the ability to accurately predict risks, especially in distinguishing those with high risks who need attention early. Reducing Disparities in Breast Cancer Diagnosis A salient benefit of the Mirai model lies in its opportunity to improve disparities in breast cancer outcomes by mitigating biases in the outcomes of traditional risk models. Traditional risk models have been proven to contain biases and have performed less accurately for various groups, including African-American and Hispanic women.
In contrast, Mirai showed consistency across both White and African-American populations in the Emory test set. This means that it is well suited for making equitable and reliable risk assessments for a diverse patient population. Having high-quality predictions of the risk of developing breast cancer with accuracy spanning a range of demographic groups allows Mirai to address the disparities present in health care for women’s care.
Current risk models, such as the Tyrer-Cuzick (TC) model, are commonly used to guide eligibility for supplemental screening, such as MRI. However, these models provide a lifetime risk assessment and fail to account for a patient’s short-term risk of developing breast cancer. This limitation has prompted researchers to seek more effective tools for predicting cancer risk within a shorter timeframe.
Mirai performs exceptionally well here as it makes predictions about risks that will develop within five years, an early window of opportunity for intervention. A retrospective analysis demonstrated that the guidelines based on Mirai had significantly better sensitivity and specificity compared to those derived from TC. Using the same level of specificity as the TC model, Mirai was able to detect 70% more patients at high risk.
When applied at the same sensitivity, it achieved a 70% relative improvement in sensitivity, which could lead to more timely and effective screenings for high-risk individuals. Although promising, the researchers note that the findings from Mirai require prospective clinical trials to be validated in clinical benefits. Retrospective analysis data is available so far, and further studies would be required to prove the real-world efficacy of the model and establish the impact on patient outcomes.
There are other significant points, which involve the reliance of the current project on Hologic mammography equipment for training and testing the model. The adaptation of Mirai for usage with other mammography vendors as well as on tomosynthesis images will become necessary for wide deployment in the future. The introduction of Mirai is an exciting milestone in breast cancer research and screening.
It can predict the risk of cancer years before clinical diagnosis, which could change the way we approach breast cancer detection, treatment, and prevention. Its ability to identify high-risk individuals more accurately than traditional methods could reduce overtreatment for those at low risk while offering more timely intervention for those at high risk. ALSO READ: Pune Reports Spike In Guillain-Barré Syndrome Cases: What You Need To Know.















