Excessive alcohol consumption is a significant public health concern, responsible for approximately 6% of all deaths and contributing to 5.1% of the global disease burden. Alcohol use is a major risk factor for over 200 diseases, including liver cirrhosis, pancreatitis, and esophageal cancer, with a particularly high incidence of gastrointestinal diseases.
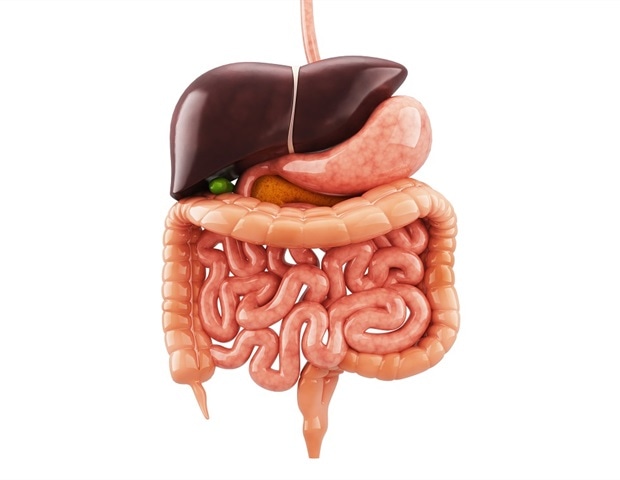
More than 50% of alcohol-related deaths are caused by gastrointestinal diseases, highlighting the importance of understanding how ethanol affects the digestive system. This review aims to provide an overview of ethanol metabolism and the diseases caused by alcohol consumption, with a focus on the liver, gastrointestinal tract, pancreas, and gallbladder. Liver The liver plays a central role in ethanol metabolism, absorbing about 90% of ingested alcohol.

Ethanol is metabolized to acetaldehyde via alcohol dehydrogenase (ADH), and acetaldehyde is further metabolized to acetate, which eventually leads to the production of carbon dioxide and water. Acetaldehyde, a highly toxic compound, can damage liver cells, causing conditions such as steatosis, steatohepatitis, alcoholic hepatitis, fibrosis, cirrhosis, and hepatocellular carcinoma (HCC). Chronic alcohol consumption accelerates liver damage, and risk factors like genetic polymorphisms and the type of alcohol consumed play important roles in disease progression.
Females, in particular, are more susceptible to alcohol-induced liver damage due to differences in alcohol metabolism and body composition. Gastrointestinal tract The gastrointestinal tract is often the first to show damage from excessive alcohol consumption, which can cause both reversible and irreversible lesions. Alcohol can lead to stomatitis, periodontal disease, and alterations in the oral microbiota.
In the esophagus, alcohol's toxic effects contribute to esophagitis, gastroesophageal reflux disease, and an increased risk of esophageal cancer, particularly when combined with smoking. Alcohol also affects gastric motility and mucosal integrity, contributing to conditions like gastritis, peptic ulcers, and eventually gastric cancer. Chronic alcohol use can impair intestinal barrier function, leading to "leaky gut," dysbiosis, and nutrient malabsorption.
These changes increase the risk of diarrhea and contribute to colorectal cancer development. Pancreas Alcohol misuse is a leading cause of pancreatitis. Acute pancreatitis (AP) and chronic pancreatitis are common consequences of alcohol consumption.
In AP, excessive alcohol intake leads to inflammation and pancreatic tissue damage, while chronic pancreatitis involves persistent inflammation, fibrosis, and pancreatic insufficiency. The pathophysiology of alcohol-induced pancreatitis is multifactorial, involving both direct toxic effects on pancreatic cells and indirect effects through the activation of inflammatory and fibrotic pathways. Pancreatic cancer is also a severe consequence of long-term alcohol abuse, with alcohol serving as a cofactor in the disease's development, particularly when combined with smoking.
Gallbladder Alcohol consumption is associated with an increased risk of gallstones and gallbladder disease. Alcohol can alter bile composition, contributing to the formation of gallstones, and chronic alcohol use can lead to gallbladder inflammation, resulting in conditions like cholecystitis. Additionally, alcohol abuse can exacerbate pre-existing gallbladder issues by increasing oxidative stress and promoting the secretion of inflammatory cytokines.
Gastrointestinal tumors Alcohol is a significant risk factor for various gastrointestinal cancers, particularly those in the esophagus, stomach, and colon. Ethanol metabolism produces acetaldehyde, a potent carcinogen that can damage DNA, inhibit DNA repair, and shorten telomeres, contributing to carcinogenesis. Alcohol consumption, particularly in combination with smoking, significantly increases the risk of esophageal squamous cell carcinoma and gastric cancer.
It is also associated with an elevated risk of colorectal cancer through mechanisms like DNA methylation induced by alcohol. Discussion Chronic alcohol consumption results in a broad spectrum of damage across the digestive system, from the oral cavity to the rectum. The severity of damage depends on factors such as the amount and frequency of alcohol intake, genetic predisposition, and the presence of other risk factors.
The interaction of alcohol with other drugs, particularly in women, can further exacerbate its harmful effects. Acetaldehyde and endotoxemia triggered by alcohol intake play critical roles in liver damage, leading to conditions like cirrhosis and liver cancer. Early detection and management of alcohol-induced damage are essential to prevent progression to more severe conditions like pancreatitis, cirrhosis, and cancer.
Conclusions Minimizing alcohol intake is crucial for digestive health. Social drinking, defined as up to one drink per day for women and two drinks per day for men, is considered the safest approach. Individuals with alcohol use disorder should seek professional support and management to reduce the risk of gastrointestinal damage.
Immediate medical evaluation is recommended for patients who present with persistent digestive symptoms linked to excessive alcohol consumption. Xia & He Publishing Inc. Caputo, F.
, et al . (2024). Effects of Ethanol on the Digestive System: A Narrative Review.
Journal of Translational Gastroenterology . doi.org/10.
14218/jtg.2024.00028 .
.















