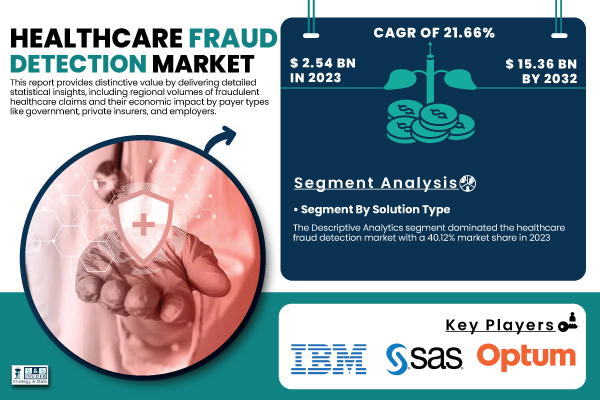
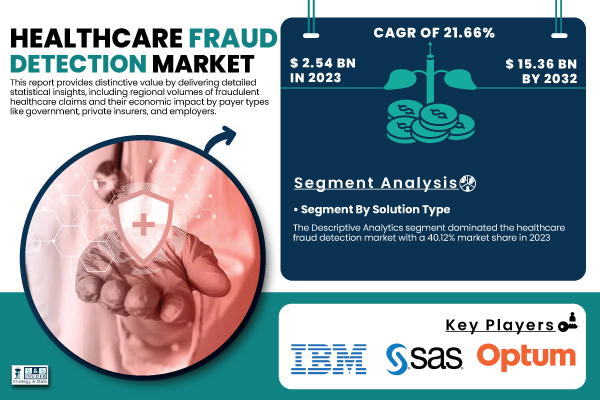
Austin, April 21, 2025 (GLOBE NEWSWIRE) -- Healthcare Fraud Detection Market Size & Growth Analysis: According to the latest report by SNS Insider, the Healthcare Fraud Detection Market , valued at USD 2.54 billion in 2023, is projected to reach USD 15.36 billion by 2032, growing at a remarkable CAGR of 21.
66% over the forecast period 2024-2032. The Healthcare Fraud Detection Market is experiencing high growth rates, stimulated by the growing incidence of healthcare fraud and increased utilization of advanced analytics solutions. Growth is propelled by the heightened sophistication of fraudulent transactions and the imperative for effective detection processes.

Get a Sample Report of Healthcare Fraud Detection Market@ https://www.snsinsider.com/sample-request/6721 The U.
S. Healthcare Fraud Detection Market was valued at USD 0.76 billion in 2023 and is expected to reach USD 4.
45 billion by 2032, growing at a CAGR of 21.29% from 2024-2032. The United States has a leading position in the North American healthcare fraud detection market, heavily dominating the region.
This dominance stems from the prevalence of high rates of fraudulent schemes like billing fraud, upcoding, and identity theft across the U.S. healthcare environment.
Public and private institutions are responding by investing heavily in sophisticated analytics and artificial intelligence-based fraud detection systems, solidifying the U.S.'s position at the center of the regional market.
Key Healthcare Fraud Detection Companies Profiled in the Report IBM Corporation (IBM Watson Health, IBM SPSS Modeler) SAS Institute Inc. (SAS Fraud Framework for Healthcare, SAS Visual Analytics) Optum, Inc. (Optum Payment Integrity, Optum Claims Manager) Conduent Inc.
(Fraud Detection Suite, PI Gateway) Change Healthcare (ClaimsXten, Payment Accuracy) EXL Service Holdings, Inc. (EXL Healthcare Analytics, EXL Payment Integrity) LexisNexis Risk Solutions (LexisNexis FraudPoint, LexisNexis ThreatMetrix) Northrop Grumman Corporation (Fraud Prevention System, Data Fusion Platform) Wipro Limited (Fraud Analytics Solution, Wipro Holmes) HCL Technologies (FRAUDWATCH, HealthEdge) Fair Isaac Corporation (FICO) (FICO Insurance Fraud Manager, FICO Falcon Platform) SCIO Health Analytics (an EXL Company) (SCIO Fraud Waste and Abuse, SCIO Claims Analytics) CTG (Computer Task Group) (Healthcare Fraud Analytics, CTG Health Solutions) DXC Technology (DXC Fraud Detection System, DXC Payment Integrity Solutions) Oracle Corporation (Oracle Healthcare Analytics, Oracle Enterprise Health Analytics) Cerner Corporation (Cerner HealtheIntent, Cerner Claims Analytics) COTIVITI, Inc. (Payment Accuracy, Risk Adjustment Solutions) Inovalon Holdings, Inc.
(Inovalon ONE Platform, Risk Adjustment Analytics) McKesson Corporation (InterQual, Clear Coverage) Allscripts Healthcare Solutions, Inc. (CareInMotion, Practice Management Analytics) Healthcare Fraud Detection Market Report Scope Segment Dynamics By Solution Type, Descriptive Analytics Segment Dominates the Market In 2023, the Descriptive Analytics segment dominated the healthcare fraud detection market with 40.12% because it plays an instrumental role in discovering historical fraud trends and billing irregularities.
This solution type allows health care organizations to review large amounts of retrospective claims and transactional data to detect anomalies like duplicate billing, upcoding, or phantom claims. Its simplicity to deliver clear and comprehensible insights without the need for advanced predictive functionality made it a popular tool with both public and private payers of healthcare. In addition, growing usage of business intelligence dashboards and data visualizations has enabled non-technical professionals to apply descriptive analytics, contributing further to its role in the healthcare industry for fraud tracking and compliance reporting.
By Delivery Mode, the On-Premises Segment Dominates the Market The On-Premises segment dominated the healthcare fraud detection market with 56.20% market share in 2023, as it exercised greater control over data security, privacy, and compliance. Health care providers and insurers dealing with sensitive patient data favored on-premises models to avoid data breach risks and violations of rules and regulations.
With this approach, confidential medical records are never kept outside of internal servers and align with severe health care norms like HIPAA in the United States. Also, sizeable healthcare organizations with strong IT infrastructures prefer on-premises installations to tailor and integrate fraud detection solutions with their legacy platforms, ensuring that they maintain confidence in fraud analytics operations being securely and locally managed. By Component, Software Segment Dominates the Market In 2023, the Software segment dominated the healthcare fraud detection market with 70.
20% market share, as the demand for sophisticated analytical software that could spot fraudulent claims in real-time grew. Software solutions make it possible to automate sophisticated data processing and integration with electronic health records (EHRs), enhancing efficiency and precision in detecting fraud. The growth of AI- and machine learning-powered platforms has further boosted predictive capabilities to enable organizations to anticipate potential fraud.
In addition, ongoing product innovation and customizable functionalities have made software solutions the pillars of contemporary fraud detection systems, especially among insurers and medical providers. By Application, Insurance Claims Review Segment Dominates the Market In 2023, the Insurance Claims Review segment dominated the healthcare fraud detection market with a 38.15% market share, primarily because of growing numbers of false insurance claims and the necessity to have stringent verification processes.
It encompasses both prepayment and postpayment review activities, allowing payers in healthcare to identify and prevent irregularities before incurring financial losses. Growing regulatory pressures on insurers to increase transparency and accuracy in the settlement of claims have also fueled demand. Furthermore, the incorporation of data analytics and artificial intelligence into claims review systems has also enhanced detection rates, leading to extensive use of these technologies by both public and private insurers.
For A Detailed Briefing Session with Our Team of Analysts, Connect with Us Now@ https://www.snsinsider.com/request-analyst/6721 Healthcare Fraud Detection Market Segmentation By Solution Type Descriptive Analytics Prescriptive Analytics Predictive Analytics By Delivery Mode On-Premises Cloud-Based By Component Services Software By Application Insurance Claims Review Postpayment Review Prepayment Review Pharmacy Billing Issue Payment Integrity Others By End-User Public & Government Agencies Private Insurance Payers Third-Party Service Providers Employers North America Dominated the Healthcare Fraud Detection Market, Asia Pacific Expected to experience the Fastest Growth North America dominated the healthcare fraud detection market with a 42.
36% market share in 2023, owing to the predominant usage of digital health technologies and the well-established healthcare infrastructure in the region. The region has a heavy workload of healthcare claims and sees high rates of fraudulent billing and coding, fueling the need for effective fraud detection systems. Asia Pacific is expected to witness the fastest growth in the healthcare fraud detection market with 22.
72% CAGR over the forecast period. This growth is driven by growing healthcare systems, increasing use of electronic health records, and heightened awareness of fraud threats in emerging economies such as India and China. Governments in the region are stepping up digitalization initiatives and imposing tighter regulations, leading providers and payers to invest in AI-based fraud analytics to minimize financial losses and enhance care integrity.
Table of Contents – Major Key Points 1. Introduction 2. Executive Summary 3.
Research Methodology 4. Market Dynamics Impact Analysis 5. Statistical Insights and Trends Reporting 5.
1 Fraudulent Healthcare Claims Volume, by Region (2023) 5.2 Cost Impact of Healthcare Fraud, by Payer Type (2023) 5.3 Detection Accuracy Rates and False Positives in Fraud Analytics Systems (2020–2032) 5.
4 Adoption Rates of Fraud Detection Solutions, by Deployment Mode (2023) 5.5 Regulatory and Compliance Enforcement Actions (2020–2023) 6. Competitive Landscape 7.
Healthcare Fraud Detection Market by Solution Type 8. Healthcare Fraud Detection Market by Delivery Mode 9. Healthcare Fraud Detection Market by Component 10.
Healthcare Fraud Detection Market by Application 11. Healthcare Fraud Detection Market by End-User 12. Regional Analysis 13.
Company Profiles 14. Use Cases and Best Practices 15. Conclusion Related Reports by SNS Insider: Artificial Intelligence in Healthcare Market Report Healthcare Claims Management Market Outlook and Trends Healthcare Predictive Analytics Market: Global Opportunities Health Insurance Exchange (HIX) Market Trends and Forecast Health IT Security Market Size and Share Analysis About Us: SNS Insider is one of the leading market research and consulting agencies that dominates the market research industry globally.
Our company's aim is to give clients the knowledge they require in order to function in changing circumstances. In order to give you current, accurate market data, consumer insights, and opinions so that you can make decisions with confidence, we employ a variety of techniques, including surveys, video talks, and focus groups around the world..
Business
Healthcare Fraud Detection Market Size to Hit USD 15.36 Billion by 2032, Driven by AI Integration and Rising Incidence of Fraudulent Claims | SNS Insider
According to Research by SNS Insider, the global healthcare fraud detection market growth is fueled by increasing fraud schemes, regulatory pressure, and demand for advanced fraud analytics solutions. According to Research by SNS Insider, the global healthcare fraud detection market growth is fueled by increasing fraud schemes, regulatory pressure, and demand for advanced fraud analytics solutions.















