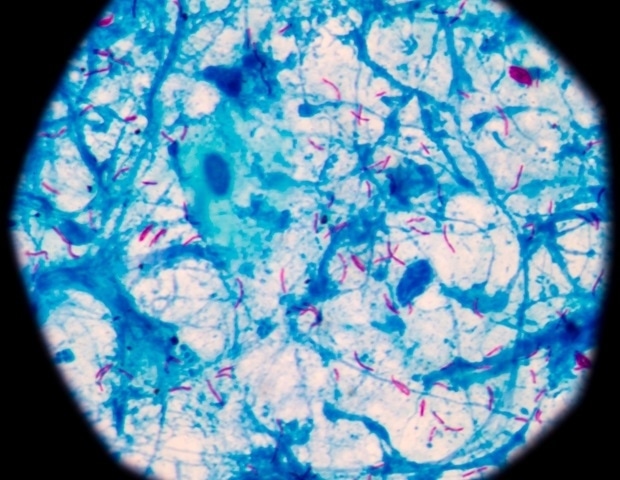
The human body hosts trillions of microorganisms, mostly friendly. More specifically, our gastrointestinal tract harbours a large number of microorganisms, most frequently bacteria, known as gut microbiome. These gut bacteria can weigh around 1 kg of our body weight.
The genetic material carried by the gut microbiome greatly outnumbers the human genes. These organisms are active participants in various processes in the body. The gut bacteria are metabolic factories of sorts, producing a large number of chemicals having a wide range of functions.

These microbiomes play a major role in generating certain enzymes necessary to synthesise vitamins such as B1, B9, B12 and K. Gut microbiome also resists the growth of pathogenic organisms (bad or disease-causing microbes) in the gut. The gut is your largest immune system organ, containing up to 80 per cent of your body’s immune cells.
Hence, these gut microbes serve an important immune function ensuring that even as we are continuously exposed to foreign particles and organisms, we still do not develop autoimmune diseases. These gut bacteria also help breaking down certain complex carbohydrates and dietary fibres that the body can’t break down on its own. While gut microbes benefit us in multiple ways, what happens when the gut dysfunctions? Gut microbiome has been a matter of considerable research in recent times and scientists call dysfunctional gut microbiome as ‘dysbiosis’.
Simply speaking, good microbes are replaced by more harmful bacteria, disrupting the balance. Additionally, reduction in diversity of gut microbes can cause many health problems. Dysbiosis has been implicated in a number of diseases, including obesity and related diseases like diabetes, fatty liver and gastrointestinal diseases like inflammatory bowel disease and irritable bowel syndrome.
And the list is ever increasing. Apart from the provision of excess calories, the signals produced by gut bacteria through chemicals modify our metabolic processes and also impact the gut barrier. So, what are the factors that can result in dysbiosis and can we prevent or cure it? The most important influence on the gut microbiome is our diet, because we are what we eat.
Studies have shown that herbivorous animals have a more diverse (healthier) gut microbiome than carnivores. Rural children have a more diverse and healthier microbiome than children living in urban areas. Broadly, a diet rich in fruits, vegetables and fibres results in a healthier gut microbiome.
On the contrary, high carbohydrate and high fat diets are likely to result in dysbiosis. The rampant use of processed and ultra-processed foods that have many food additives and emulsifiers adversely impacts the gut microbiota. Lifestyle diseases like obesity, diabetes, fatty liver, and gastrointestinal diseases like inflammatory bowel disease and irritable bowel syndrome have been blamed largely on the changing dietary practices.
The changing lifestyles and diet have resulted in the disruption of gut health, causing an increase in these diseases. Diet influences our gut health through changes in the gut microbiota. It is, therefore, not surprising that dietary therapies which focus on changing gut microbiota have been found to be useful in many of these diseases.
In particular, the Mediterranean diet that emphasises increased intake of fruits, legumes, nuts, whole grains and vegetables and exclusion of animal fats, sweets and processed food seems to work in many of these diseases. While change in the diet is certainly an important intervention to improve our gut microbiome, there are other approaches also. Prebiotics like inulin, fructoligosaccharides (found in onion, leeks, asparagus, etc) or prebiotic-rich foods (banana, garlic, apples and legumes) are also known to promote the growth of health-promoting organisms.
Commercial preparations of health promoting strains of microorganisms are available as probiotics. While these may be helpful in the short term, their effect is not believed to be long lasting. In addition, these are obviously costlier.
The long-term solution is to modify our diet. Another interesting approach has been the use of faecal transplants. In this, the stool of healthy individuals is transplanted in individuals with compromised gut health to change their gut microbiome.
These changes are believed to be long lasting. While faecal transplants are currently approved only for a specific infectious form of antibiotic-associated diarrhoea, they are an area of active research in many diseases. The future is likely to witness a number of therapeutic strategies that focus on gut health, including the use of bioengineered products.
Till then, a healthy diet seems to be the best approach to improve our gut microbiome and gut health. The writer is additional professor, gastroenterology, PGI, Chandigarh.
Health
Healing the gut
The human body hosts trillions of microorganisms, mostly friendly. More specifically, our gastrointestinal tract harbours a large number of microorganisms, most frequently bacteria, known as gut microbiome. These gut bacteria can weigh around 1 kg of our body weight. The genetic material carried by the gut microbiome greatly outnumbers the human genes. These organisms are [...]