To better understand why some cancer patients struggle to fight off infections, Georgia Tech researchers have created tiny lab-grown models of human immune systems. These miniature models -; known as human immune organoids -; mimic the real-life environment where immune cells learn to recognize and attack harmful invaders and respond to vaccines. Not only are these organoids powerful new tools for studying and observing immune function in cancer, their use is likely to accelerate vaccine development, better predict disease treatment response for patients, and even speed up clinical trials.
Our synthetic hydrogels create a breakthrough environment for human immune organoids, allowing us to model antibody production from scratch, more precisely, and for a longer duration." Ankur Singh, Carl Ring Family Professor in the George W. Woodruff School of Mechanical Engineering and professor in the Wallace H.
Coulter Department of Biomedical Engineering at Georgia Tech and Emory "For the first time, we can recreate and sustain complex immunological processes in a synthetic gel, using blood, and effectively track B cell responses," he added. "This is a gamechanger for understanding and treating immune vulnerabilities in patients with lymphoma who have undergone cancer treatment -; and hopefully other disorders too." Led by Singh, the team created lab-grown immune systems that mimic human tonsils and lymph node tissue to study immune responses more accurately.
Their research findings, published in the journal Nature Materials , mark a shift toward in vitro models that more closely represent human immunology. The team also included investigators from Emory University, Children's Hospital of Atlanta, and Vanderbilt University. Designing a tiny immune system model The researchers were inspired to address a critical issue in biomedical science: the poor success rate of translating preclinical findings from animal models into effective clinical outcomes, especially in the context of immunity, infection, and vaccine responses.
"While animal models are valuable for many types of research, they often fail to accurately mirror realistic human immune biology, disease mechanisms, and treatment responses," said Monica (Zhe) Zhong, a Bioengineering Ph.D. student and the paper's first author.
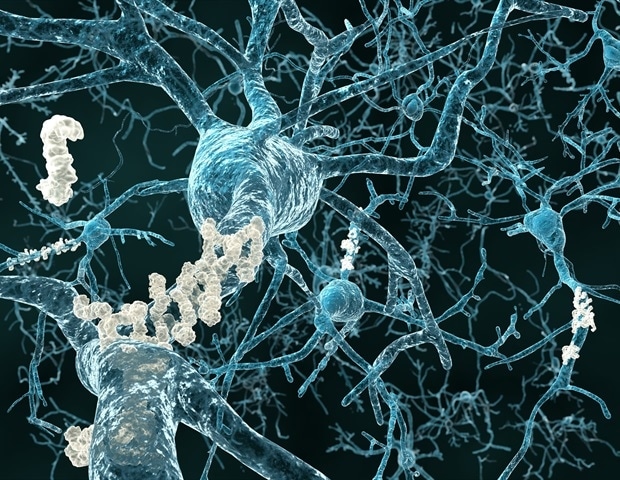
"To address this, we designed a new model that faithfully replicates the unique complexity of human immune biology across molecular, cellular, tissue, and system levels." The team used synthetic hydrogels to recreate a microenvironment where B cells from human blood and tonsils can mature and produce antibodies. When immune cells from healthy donors or lymphoma patients are cultured in these gel-like environments, the organoids support longer cell function, allowing processes like antibody formation and adaptation to occur -; similar to the human body.
Utilizing the organoids for individual patients helps predict how that individual will respond to infection. The models also enable researchers to control and test immune responses under various conditions. The team discovered that not all tissue sources are the same, and tonsil cells struggled with longevity issues.
They used a specialized setup to study how healthy immune cells react to signals that help them fight infections, which failed to trigger the same response in cells from lymphoma survivors who seemingly have recovered from immunotherapy treatment. Related Stories How physical activity before and after cancer treatment improves outcomes Researchers develop new antibody with potential to treat several types of cancer Novel bladder cancer treatment gains MHRA approval in the UK Using organoids embedded in a novel immune organ-on-chip technology, the team observed that immune cells from lymphoma survivors treated with certain immunotherapies do not organize themselves into specific "zones," the way they normally would in a strong immune response. This lack of organization may help explain some immune challenges cancer survivors face, as evidenced by recent clinical findings.
A game-changing technology This research is primarily of interest to infectious disease researchers, cancer researchers, immunologists, and healthcare professionals dedicated to improving patient outcomes. By studying these miniature immune systems, they can identify why current treatments may not be effective and explore new strategies to enhance immune defenses. "Lymphoma patients treated with CD20-targeted therapies often face increased susceptibility to infections that can persist years after completing therapy.
Understanding these long-term impacts on antibody responses could be key to improving both safety and quality of life for lymphoma survivors," said Dr. Jean Koff, associate professor in the department of Hematology and Oncology at Emory University's Winship Cancer Institute and a co-author on the paper. "This technology provides deeper biological insights and an innovative way to monitor for recovery of immunological defects over time.
It could help clinicians better identify patients who would benefit from specific interventions that reduce infection risk," Koff added. Another critical and promising aspect of the research is its scalability: An individual researcher can make hundreds of organoids in a single sitting. The model's capability to target different populations -; both healthy and immunosuppressed patients -; vastly increases its usability for vaccine and therapeutic testing.
According to Singh, who directs the Center for Immunoengineering at Georgia Tech, the team is already pushing the research into new dimensions, including developing cellular therapies and an aged immune system model to address aging-related questions. "At the end of the day, this work most immediately affects cancer patients and survivors, who often struggle with weakened immune responses and may not respond well to standard treatments like vaccines," Singh explained. "This breakthrough could lead to new ways of boosting immune defenses, ultimately helping vulnerable patients stay healthier and recover more fully.
" The work was initially funded by the Wellcome Leap HOPE program. This support has led to a boost in recent funding, including a recent $7.5M grant from the National Institute of Allergy and Infectious Diseases.
Georgia Institute of Technology Zhong, Z., et al . (2024).
Human immune organoids to decode B cell response in healthy donors and patients with lymphoma. Nature Materials . doi.
org/10.1038/s41563-024-02037-1 ..