The ear, which consists of the outer, middle, and inner parts, can become infected by bacteria, fungi, or viruses in the ear canal or eustachian tube, affecting its ability to transmit and process sound. The main types of ear infections include: Vertigo: Symptoms, Causes, Treatments, and Natural Approaches Ménière’s Disease: Symptoms, Causes, Treatments, and Natural Approaches Acute otitis media: Signs and symptoms of infection lasting up to six weeks Subacute otitis media: Symptoms lasting between six weeks and three months Otitis media with effusion: Fluid in the middle ear without signs and symptoms of infection Less Common Types of Ear Infections Viral infections may directly cause ear infections or create conditions that make the ear more vulnerable to secondary bacterial infections. Causes by Specific Infection Types Bacterial overgrowth: Most commonly caused by Pseudomonas aeruginosa or Staphylococcus aureus, especially in moist environments.
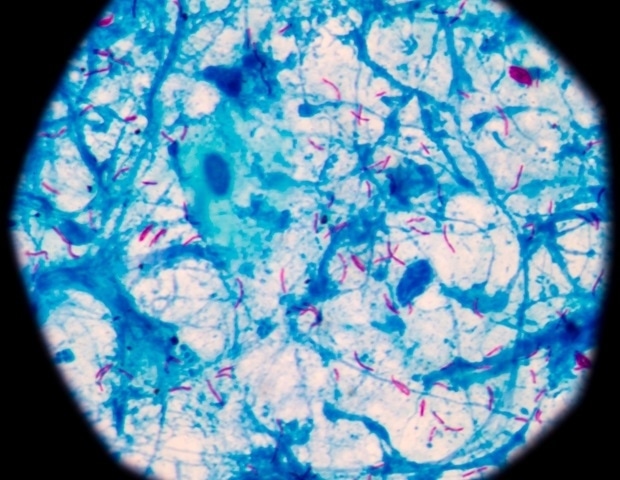
Fungal presence: Species like Candida and Aspergillus can sometimes grow in the ear canal, often after prolonged moisture exposure or antibiotic use. Ear canal trauma: Scratching, use of cotton swabs, or inserting foreign objects can damage the skin and allow pathogens to enter. Obstructed ear canal: Earwax buildup can trap moisture and create a breeding ground for microbes.

Eustachian tube dysfunction: Blocked or poorly functioning tubes prevent fluid from draining properly, allowing pathogens to multiply. Bacterial infection: Often caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Enlarged or infected adenoids: Can block the eustachian tubes and harbor bacteria.
Mucus overproduction: Can lead to fluid accumulation behind the eardrum, especially in teething infants. Viral or bacterial invasion: Infections such as maternal rubella, cytomegalovirus (in newborns), or complications from bacterial meningitis may reach the inner ear. Autoimmune response: Conditions like polyarteritis nodosa and granulomatosis with polyangiitis can trigger inflammation in the inner ear structures.
Vestibular nerve involvement: Viruses affecting the vestibular nerve can lead to inner ear inflammation and disrupt balance. Risk Factors Environmental factors also play a critical role, with exposure to tobacco smoke emerging as a significant contributor. Tobacco smoke can cause inflammation and increase susceptibility to infection.
A personal medical history of previous ear infections can further compound risk, as prior ear problems often indicate increased biological vulnerability to future complications. Unique Risk Factors by Infection Type Swimming: Especially in contaminated water, which introduces bacteria into the ear canal (associated with a fivefold increase in risk). Humidity: Warm, moist environments promote bacterial and fungal growth in the ear canal.
Narrow ear canals: Reduced airflow and drainage can lead to moisture buildup. Chronic conditions: Skin issues such as diabetes, eczema, and dermatitis can impair the ear’s natural defenses. Hearing aid use: Devices may cause irritation and trap moisture in the ear canal.
Chemical irritants: Shampoos, hair products, and certain ear care items can disrupt the skin barrier or cause inflammation. Age: Children between 6 and 12 months have smaller, more horizontal eustachian tubes, making them more prone to fluid buildup and infection. Premature birth: Babies born before 37 weeks of gestation may have underdeveloped ear structures and immune defenses.
Sex: Otitis media is slightly more common in boys and men. Bottle feeding: Drinking from a sippy cup or bottle while lying down may have milk allow fluid to enter the eustachian tube. Lack of breastfeeding: Breast milk contains protective antibodies, so not breastfeeding may reduce children’s natural defenses.
Pacifier use: Linked to increased pressure changes and bacterial transfer in the middle ear. Daycare attendance: Raises exposure to viruses and bacteria, especially in group care settings. Cleft palate: Can disrupt normal eustachian tube function and drainage.
Down syndrome: Often associated with structural and immune differences that affect ear health. Indigenous heritage: Children of First Nations and Inuit descent face higher risk, though the reasons are not fully understood. Family history: A strong genetic component may influence susceptibility.
Recent viral respiratory infection: Colds and other illnesses can lead to inflammation and fluid buildup in the middle ear. Age: Viral labyrinthitis is most common in adults between 30 to 60, while bacterial cases more often affect children under 2. Viral history: Prior infections such as herpes, measles, mumps, polio, hepatitis, Epstein-Barr virus, or varicella may contribute.
Excessive alcohol use: Linked to inner ear inflammation, particularly in cases of labyrinthitis. Chronic otitis media: Long-standing middle ear problems can progress to inner ear involvement. Many also experience a feeling of fullness inside the ear, along with noticeably reduced hearing, which may be described as muffled or partially lost.
Unique Symptoms by Condition Otitis externa: Tenderness when touching the tragus or pinna Itching or irritation in and around the ear canal Redness and swelling of the outer ear or ear canal Flaky or peeling skin around the ear canal Swollen or sore glands in the neck or throat Pain that worsens while chewing A squelching or popping sensation when moving the ear or jaw Otitis media: Nasal congestion Cough Lethargy or low energy Vomiting Loss of appetite Fluid drainage or a ruptured eardrum Otitis interna: Vertigo or a sensation of dizziness or the room spinning Difficulty maintaining balance Nausea and vomiting Ringing or buzzing in one or both ears Involuntary, rapid eye movements Mild headaches Unique Symptoms in Infants and Young Children Following the medical history review, a physical examination is conducted to assess the ears and surrounding areas. Type-Specific Diagnostic Approaches Diagnosis is based on visible inflammation in the ear canal, especially when the tragus or pinna is tender. In some cases, if the infection is recurrent or the patient is immunocompromised, a drainage sample may be collected to identify bacterial or fungal causes.
Doctors look for a bulging or inflamed eardrum or fluid behind it. Hearing tests may be used in patients with a history of infections. Tympanometry and tympanocentesis help assess middle ear pressure and fluid.
Infants under 12 weeks with fever may need a full sepsis workup. The most immediate risk involves hearing. Patients may experience partial or complete hearing loss or develop persistent tinnitus—a condition characterized by chronic ringing or buzzing in the ears.
In more extreme scenarios, ear infections may trigger neurological complications. Facial nerve paralysis can impair muscle control, resulting in both cosmetic and functional challenges. Untreated infections can also spread to the central nervous system, potentially leading to severe conditions like bacterial meningitis—a dangerous inflammation of the protective membranes surrounding the brain and spinal cord.
Another serious risk is a brain abscess, where a localized infection forms a pocket of pus within brain tissue. Complications by Infection Type Outer ear complications: Malignant otitis externa: A life-threatening infection typically affecting older adults with diabetes or immunocompromised patients Auricular or periauricular cellulitis: Bacterial infection of the skin and tissues around the outer ear Perichondritis : Infection of the cartilage in the outer ear Myringitis: Inflammation of the eardrum Facial cellulitis: Bacterial skin infection affecting the face Osteomyelitis of the temporal bone: A serious bone infection that can spread from the ear Middle ear complications Serous otitis media: Persistent fluid buildup without infection Eardrum perforation: Acute and chronic tearing of the eardrum Cholesteatoma: Abnormal skin growth in the middle ear Tympanosclerosis: Scarring or calcification of the eardrum Petrositis: Infection of the temporal bone; rare but sometimes fatal Cholesterol granuloma: Cyst-like lesion at the skull base near the middle ear Infectious eczematoid dermatitis: Inflammatory skin condition affecting the ear canal Subdural empyema: Collection of pus between the brain and its outer membrane Extradural abscess: Infection between the skull and the brain’s outer covering Otitic hydrocephalus: Increased intracranial pressure related to chronic middle ear infection Inner ear complications Bilateral vestibular hypofunction: A severe condition often caused by bacterial meningitis. It can lead to blurred vision during movement (oscillopsia) and problems with balance and spatial awareness.
Labyrinthitis ossificans: This is when the inner ear structures harden as they gradually turn to bone, potentially leading to permanent hearing or balance loss. Benign paroxysmal positional vertigo: This condition affects 10 to 15 percent of patients within a few weeks of onset. Persistent postural-perceptual dizziness: A form of chronic, nonspinning vertigo and unsteadiness that affects up to 25 percent of those diagnosed.
Pain management is a key component of early treatment. Over-the-counter pain relievers are commonly recommended to ease discomfort across various types and severities of infection. Ear hygiene is also important, particularly for outer ear infections.
Doctors often advise keeping the ear dry, as moisture can worsen symptoms and delay healing. Some cases may be managed with a watchful waiting approach, giving the immune system two to three days to fight the infection without medical intervention. While this is more common in some countries, it’s less widely practiced in the United States, where more proactive treatment is often preferred.
Treatments by Infection Type Corticosteroid ear drops: Helps reduce inflammation Topical antibiotic ear drops: Commonly prescribed; oral antibiotics are rarely needed Acetic acid (vinegar) ear drops: Create an acidic environment that inhibits bacterial growth Warm compress: Applying a warm cloth to the ear may help if a boil is present Professional ear cleaning: Recommended in cases of acute otitis externa Homecare: Apply a warm cloth to the affected ear, stay hydrated, and avoid allergens such as dust Observation (watchful waiting): Often recommended with close follow-up Oral antibiotics: Prescribed based on clinical guidelines, especially in more severe or prolonged cases Myringotomy: A small surgical incision in the eardrum may be considered in cases of significant pain, fever, or persistent symptoms—though this is rarely performed Adenoid removal surgery: Enlarged adenoids contributing to recurring ear infections may be removed; however, tonsil removal does not help prevent ear infections Labyrinthitis treatment: Depends on the cause and may include rest, hydration, antiviral medications, corticosteroids, or immunomodulators such as azathioprine, etanercept, or cyclophosphamide Symptom relief: Short courses of benzodiazepines or antihistamines may reduce vertigo; antiemetics like prochlorperazine can ease nausea Antibiotics: Rarely used unless a bacterial cause is confirmed Surgery: Considered in a small number of cases Physical therapy: Vestibular rehabilitation may help the brain adapt to changes in balance signals A positive outlook may support immune function, reduce stress, and improve pain tolerance, potentially aiding recovery. Herbal Medicines Herbal remedies like Sinupret and mullein have traditionally been used to support upper respiratory and ear health. Sinupret is a German formula made from plant extracts such as sorrel, European elder, cowslip, European vervain, and gentian root.
It may help relieve sinus congestion, which can indirectly reduce ear pressure and discomfort. Mullein (Verbascum), commonly used in Spanish folk medicine, has a long history of use for earaches and ear infections. While both remedies are widely used in traditional practice, scientific evidence supporting their effectiveness remains limited.
Propolis-Based Products Homeopathy Vitamin D Supplements Xylitol Products Avoid scratching the inside of your ears or inserting objects like cotton swabs Keep ears clean and dry, especially while showering or bathing Avoid swimming in dirty or polluted water After getting wet, dry your ears thoroughly by tilting your head to drain excess water or using a hairdryer on low heat and lowest speed setting at least a foot away from the ear Use earplugs when swimming, particularly in pools or lakes with questionable water quality Consider using a mixture of rubbing alcohol and white vinegar after swimming to help prevent bacterial growth. Consult a health care provider for proper preparation, dosage, and application Avoid smoking and exposure to secondhand smoke Wash hands frequently—yours, theirs, and their toys—to limit the spread of germs If possible, breastfeed infants and avoid bottle-feeding while they are lying down Transition from a bottle to a cup by age one, and never put them to bed with a bottle Reduce pacifier use after six months, as prolonged use may increase the risk of infection Keep children away from secondhand smoke Choose smaller daycare settings, when possible, to minimize exposure to infections Protect their ears by keeping them dry when swimming by using earplugs or a bathing cap Treat underlying ear-related conditions such as eczema or allergies Limit their contact with sick children when possible.