Bacterial vaginosis (BV), affecting more than three million women in the United States each year, is, in fact, a sexually transmitted infection (STI), according to a new study from Australia. The new understanding, built on decades of research, represents a major shift in how we approach BV and its treatment, offering new possibilities for women affected by its recurrent symptoms, such as discharge, itching, and inflammation, as well as serious risks like infertility, premature birth, and newborn deaths. “We’ve proven that reinfection [from partners] is driving a significant portion of recurrence—in fact, the majority,” Catriona Bradshaw, a clinician-researcher who co-led the study, told The Epoch Times.
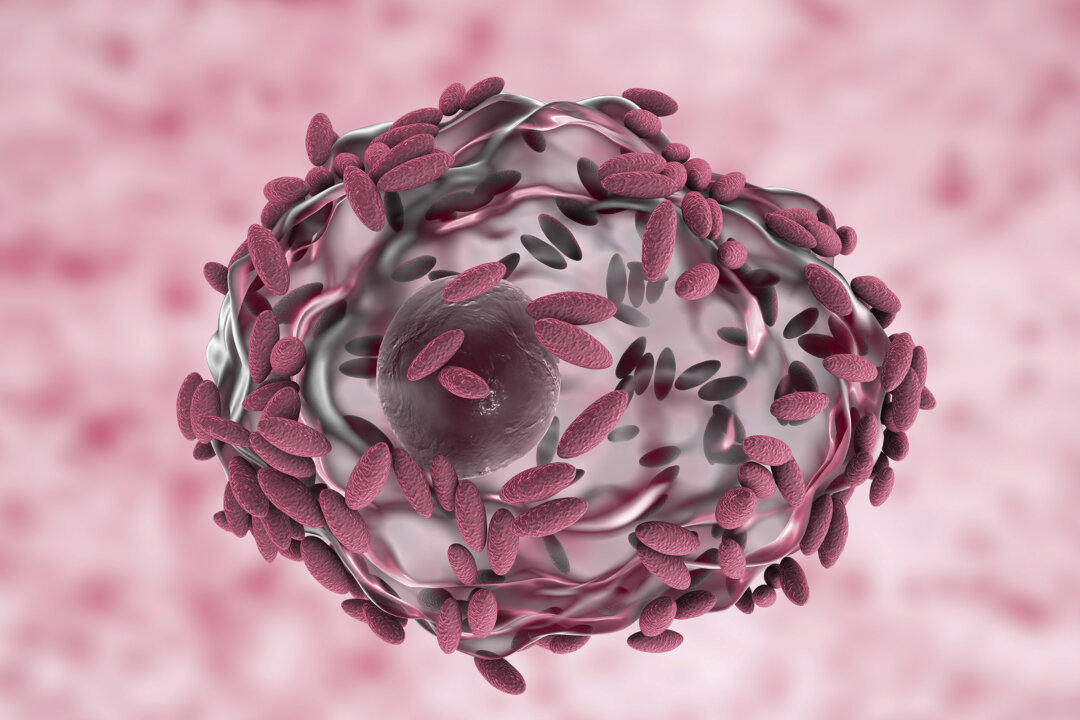
In a healthy vagina, Lactobacillus bacteria protect against infections and support healthy pregnancies. However, in BV, these beneficial bacteria are replaced by a mix of harmful microbes, including Gardnerella, Atopbium, and Mobiluncus bacteria. Treating BV as a simple vaginal imbalance, meaning that only the female is treated with antibiotics, rather than as an STI, where both partners receive treatment, may be why more than half of women experience recurrence within three months, Lenka Vodstrcil, co-lead researcher, told The Epoch Times.

Women whose partners also received the one-week treatment of the oral antibiotic metronidazole with the addition of topical clindamycin cream for men to apply their genital areas had a recurrence rate of only 35 percent, compared to 63 percent in the control group, which included only the women being treated for the infection. All participants were selected for having a high burden of risk factors for BV recurrence. Eighty-seven percent of women had a history of recurring BV, and 80 percent of men were uncircumcised—known to increase the risk of BV transmission due to potential bacterial buildup.
Additionally, one-third of the women used intrauterine device (IUD) birth control, which can provide a surface for bacteria to adhere to, making infections more persistent and harder to treat, the researchers noted. Advances in molecular technology have further supported this theory, revealing that the bacteria responsible for BV are also present on penile skin and in the urethra of men, which helps explain why BV-causing bacteria are exchanged between partners, leading to high recurrence rates after treatment. Bradshaw notes that many clinicians have long suspected BV is an STI, given its association with sexual activity, such as changing partners and inconsistent condom use.
BV often develops within days to weeks after sexual contact, making it similar to other STIs in terms of its timing after exposure. Bradshaw suggests that the conclusions of these studies may be affected by potential biases, particularly in face-to-face interviews with 16-year-old girls. She raises the possibility that the gender of the interviewers, often male gynecologists, could have influenced the girls’ willingness to disclose sexual activity.
Bradshaw designed a study using anonymous questionnaires and self-collected samples from university students. The results revealed a clear pattern: Women with no sexual activity had no BV; those with non-penetrative sexual activities had a small amount; and women who had engaged in penetrative sex had significantly higher rates of BV. Some women may be less responsive to treatment—those with copper IUDs are at a higher risk of BV recurrence.
While adjunct therapies like probiotics may support the gut microbiome, there’s limited evidence that they benefit the vaginal microbiome. However, a specific probiotic called LACTIN-V, a vaginal lactobacillus species, has shown promise. However, reinfection, in most cases, is primarily driven by the presence of an infected partner, according to Vodstrcil and Bradshaw.
“The external partner is still there, and sexual activity can disrupt the balance,” Vodstrcil says, highlighting the importance of treating both partners—not just with antibiotics but with topical cream for men as well. Untreated male partners still harbor the bacteria responsible for BV, leading to reinfection in women. This shift in understanding could lead to updates in global health guidelines, including recommendations for condom use to help prevent both getting BV and having it recur, Vlodstrcil said.
The website features links to the study and participants’ experiences. It also includes information on side effects, such as nausea, headaches, and a metallic taste—common with antibiotics. Additionally, the site provides simple labeling instructions for pharmacists, who will need to repackage the clindamycin cream as a product men can also use.
.















