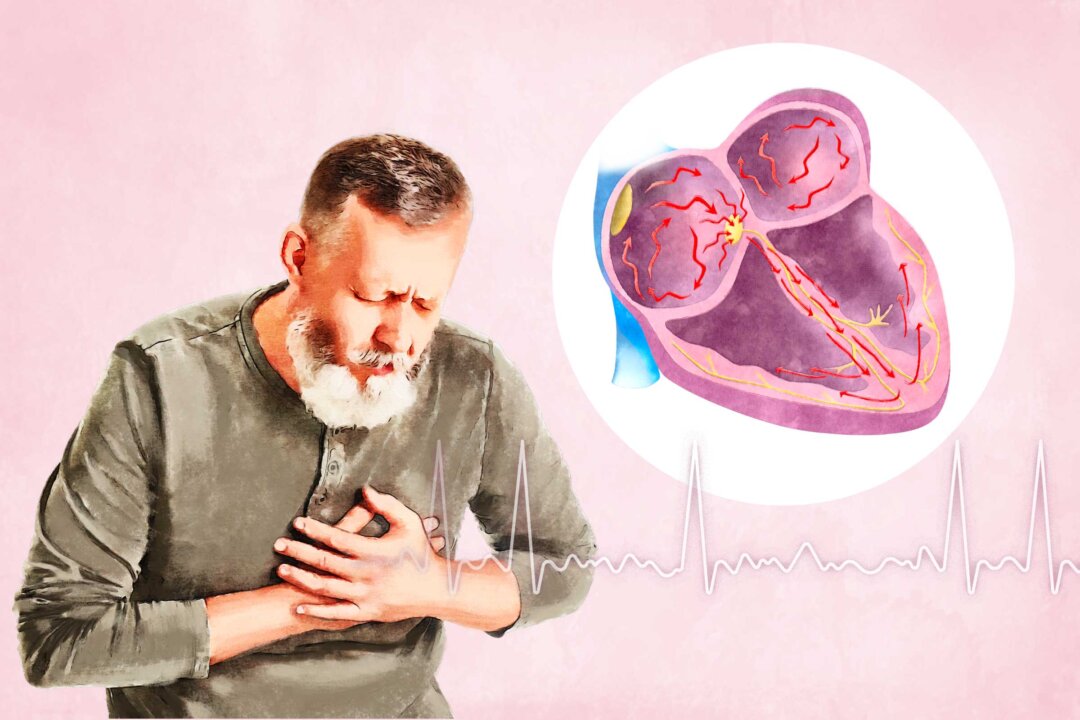
Atrial fibrillation, often referred to as “A-fib,” is an electrical disorder in the heart’s upper chambers that causes an abnormal heart rhythm (arrhythmia) and disrupts the normal flow of blood between the upper and lower chambers. Left untreated, A-fib can lead to serious complications, including blood clots, stroke, and heart failure. A-fib symptoms vary from person to person.
Common symptoms include: Heart palpitations (rapid, fluttering, or pounding heartbeat) Low energy or fatigue Shortness of breath Trouble exercising or performing everyday activities Lightheadedness or dizziness Fainting Low blood pressure Fluid buildup in the legs, ankles, or feet Blood clots Chest discomfort, pain, or tightness Mitral Valve Prolapse: Symptoms, Causes, Treatments, and Natural Approaches Aortic Stenosis: Symptoms, Causes, Treatments, and Natural Approaches The heart has four chambers: two upper chambers, called the atria, and two lower chambers, called the ventricles. Electrical impulses travel along a pathway in the heart, signaling the atria and ventricles to work harmoniously to pump blood through the heart and into the body. In a healthy heart, a heartbeat begins with an electrical impulse to a tiny bundle of tissue in the right atrium called the sinoatrial (SA) node.

This electrical impulse causes both atria to contract and pump blood down to the ventricles. The electrical current continues to travel through another bundle of tissue called the atrioventricular (AV) node, triggering the ventricles to contract and then relax in a steady rhythm. In A-fib, the electrical signals in the atria become disorganized, causing the upper chambers to quiver or fibrillate.
These chaotic signals continue to flood the AV node as they try to reach the ventricles, resulting in a rapid and irregular heart rhythm. Medical Conditions Congenital heart defect: Structural abnormalities that affect the heart’s electrical system Heart valve disease: Leaking (regurgitation) or stenotic (narrowed) heart valves that enlarge heart chambers and interfere with electrical impulses Coronary artery disease: Restricted blood supply to the heart, leading to tissue damage and electrical instability Sleep apnea: Disrupted breathing patterns during sleep that strain the heart muscle and affect electrical pathways Sinus node dysfunction: Malfunctioning of the sinus node, a natural pacemaker, that causes the heart’s upper chamber or atria to twitch rather than contract normally Health Problems Heart attack High blood pressure Overactive thyroid (hyperthyroidism) Lung infections, such as pneumonia Viral infections Lifestyle Factors Using illegal drugs Drinking excessive alcohol or caffeine Smoking Taking stimulant-containing cold and allergy medications Paroxysmal A-fib Persistent A-fib Long-Standing Persistent A-fib Permanent A-fib Stage 1: At Risk for A-fib Risk factors such as lifestyle, weight, and diabetes may be controllable, while others, such as age or genetics, are not. Stage 2: Pre-A-fib The heart shows early signs of electrical changes that could lead to A-fib.
Treatment and closer monitoring begin to prevent progression. Stage 3: Diagnosed A-fib A formal diagnosis is made. Treatment focuses on controlling heart rate and rhythm with medications, procedures, or both.
Stroke risk increases, so blood thinners may be recommended. Stage 4: Permanent A-fib A-fib persists despite treatment. Management focuses on symptom control and regular stroke risk assessment.
Age: A-fib becomes more common with age, affecting about 70 percent of people with irregular heart rhythms between 65 and 85. Family history: Certain genetic mutations can increase the likelihood of developing A-fib. Medical conditions: Heart, lung, and sleep disorders can contribute to irregular heart rhythms.
Race: A-fib is more common in white people of European descent. Stress or panic disorders: Chronic stress or anxiety can trigger irregular heartbeats. Unhealthy habits: Smoking, excessive alcohol consumption, and illegal drug use can strain the heart and increase A-fib risk.
Obesity: Excess weight puts added stress on the heart and may contribute to electrical disturbances. Surgical procedures: Surgeries involving the heart, lungs, or esophagus can affect heart rhythm. Chronic kidney disease: Reduced kidney function is linked to a higher risk of A-fib.
Heart valve disease: Leaking or narrowed heart valves can lead to irregular heart rhythms. High blood pressure: Increased pressure forces the heart to work harder, which can contribute to A-fib. Diabetes: High blood sugar levels can damage blood vessels and increase A-fib risk.
Hyperthyroidism: An overactive thyroid can overstimulate the heart, leading to irregular rhythms. Sleep apnea: Interrupted breathing during sleep can strain the heart and affect its electrical system. Chronic obstructive pulmonary disease (COPD): Lung disease can lead to reduced oxygen levels and increased heart strain.
Basic Diagnostic Tests Electrocardiogram (EKG): Records the heart’s electrical activity and can detect A-fib if it occurs during the test Holter monitor: A portable EKG worn for days or weeks to catch irregular heart rhythms that occur intermittently. Loop recorder: A small implanted device that continuously tracks heart rhythm over months or years Imaging Tests: Echocardiogram: An ultrasound of the heart that evaluates chamber size, pumping function, and possible blood clots Chest X-ray: Helps detect an enlarged heart or fluid buildup in the lungs Cardiac magnetic resonance imaging: Produces detailed images of the heart’s structure and function to assess abnormalities Other Assessments: Blood tests: Measures thyroid function and checks for other conditions that may contribute to A-fib Sleep study: Identifies sleep apnea, a common trigger for A-fib Exercise stress test: Evaluates how the heart responds to physical activity and detects abnormalities that may not appear at rest Stroke Heart Failure Dementia Control heart rate and rhythm Prevent blood clots and reduce stroke risk Restore the heart to a normal rhythm Address underlying conditions and complications Reduce risk factors that can worsen A-fib Medications Rate control medications: Slow the heart rate and prevent the heart muscle from weakening. Examples include: beta-blockers such as metoprolol and atenolol Rhythm control medications: Also called anti-arrhythmic drugs, these help maintain a regular heart rhythm Blood thinners: Also called anticoagulants, help prevent blood clots and reduce the risk of stroke More Invasive Procedures Electrical cardioversion: A procedure that involves using a controlled electrical shock through a defibrillator to reset the heart’s rhythm.
If A-fib is severe, cardioversion may be performed immediately. Otherwise, doctors usually wait three to four weeks after starting blood thinners to reduce the risk of stroke from potential clots. Blood thinners are continued for at least four weeks after the procedure.
Catheter ablation: A minimally invasive procedure in which a doctor inserts a thin, flexible tube (catheter) into a blood vessel in the groin and guides it into the heart. Heat or cold energy is used to create small scars in the heart tissue, disrupt the irregular electrical pathways in the heart, and help restore a normal rhythm. Catheter ablation can sometimes cure A-fib altogether.
Maze Procedure: Performed during open-heart surgery, this procedure involves creating scar tissue in the heart using a scalpel. The scars disrupt abnormal electrical signals. Many people planning a coronary bypass or heart valve surgery also receive a Maze procedure.
Left atrial appendage closure: A procedure that seals off a small sac in the heart’s upper left chamber where blood clots often form. A closure device is advanced through a catheter to the left atrial appendage, where it remains permanently. Alternative Therapies Yoga therapy: This has been shown to promote general health and well-being and positively affect many chronic medical conditions.
Yoga can also play a key role in treating A-fib due to its impact on the autonomic nervous system. Studies suggest that yoga may help lower resting heart rate, reduce A-fib triggers, and decrease stress and oxidative damage that contribute to heart muscle changes. Acupuncture: Although studies are limited, one trial assessed how effective acupuncture was for restoring normal heart rhythm (cardioversion) in A-fib patients.
Researchers found that 85 percent of patients achieved cardioversion with acupuncture compared to 67.5 percent of those treated with the anti-arrhythmic drug amiodarone. A 2017 review of 13 randomized controlled trials suggested that acupuncture can help restore normal heart rhythm and improve recovery time.
Biofeedback: This therapy uses a monitor to show heart rate or breathing patterns. Patients practice relaxation techniques like deep breathing to help slow their heart rate. Although a small study in 1973 showed potential benefits for A-fib, biofeedback is not yet widely used for this condition.
Herbal Medicines Health Factors Cholesterol levels: Keeping cholesterol within a healthy range reduces heart strain. Blood pressure: Managing blood pressure helps prevent heart damage. Blood glucose: Controlling blood sugar levels lowers the risk of heart-related complications.
Behavioral Factors S moking : Avoiding cigarettes reduces inflammation and heart strain. Physical activity: Regular exercise strengthens the heart and improves circulation. Diet: A heart-healthy diet supports overall cardiovascular function.
Body mass index: Maintaining a healthy weight helps reduce heart disease risk. Simple Steps to Help Prevent Atrial Fibrillation Exercise for at least 30 minutes per day, or as tolerated Limit alcohol intake Stop smoking Eat a heart-healthy diet Maintain a healthy weight Treat underlying conditions such as hypertension, heart valve disease, and atherosclerosis.















